How Healthcare Systems Can Bolster Hospital Resilience
Extreme weather is becoming more frequent and intense, posing major challenges to healthcare system operations.
Hospitals are required to maintain emergency back-up systems. Still, critical infrastructure remains vulnerable in the face of unprecedented disasters. Diesel generators and conventional back-up equipment are not designed for prolonged use, and they typically serve only a portion of campus facilities.
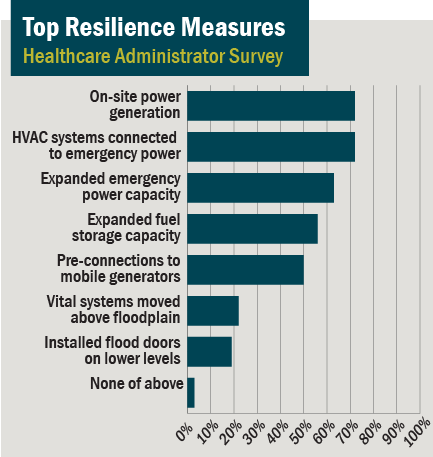
In response, a growing number of hospitals are going above and beyond minimum code requirements, investing in resilience measures that enable uninterruptible operations.
Extreme Weather’s Perilous Impacts
Hospitals must prepare for an increasingly uncertain future. Rising temperatures are anticipated to produce more extreme weather, heightening existing risks or creating entirely new climate-related vulnerabilities.
Recent disasters have demonstrated the potential of massive financial losses. In 2012, Hurricane Sandy hammered New York with $3 billion in healthcare facility damages — based on initial, likely under-reported estimates. In 2017, Hurricane Harvey swept across Texas, leaving hospitals with $420 million in recovery costs.
Many hospitals are becoming more proactive by evacuating patients before major storms make landfall. A study of coastal hospitals found evacuation-related expenses and revenue losses can total $9.5 million with each incident.
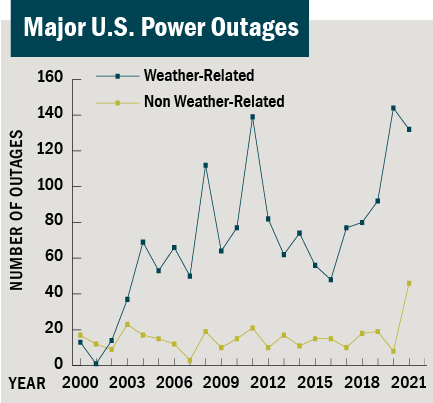
Source: Climate Central
Common Hospital Infrastructure Vulnerabilities
Burns’ healthcare clients are expressing greater concerns over whether their facilities can handle the impact of more-extreme weather — in particular, severe storms and flooding events. Even temporary disruption to critical electricity, gas, steam, water, or fiber-optic utilities can have far-reaching and perilous implications.
Without new resilience measures, hospital building systems and central utilities may be inadequate during times when they are needed most. Hospitals are required to maintain essential systems’ power supplies for, at minimum, 96 hours. Yet disruption to “non-critical” systems — such as air conditioning or certain medical communications — can still undermine basic patient-care services.
Common hospital infrastructure vulnerabilities include:
- Infrastructure systems operating well beyond life expectancy
- Risk of back-up generator failure due to poor equipment maintenance or susceptibility to flooding
- Limited back-up supplies, especially when inefficient use of resources increases the total supplies necessary to maintain hospital operations
- Critical hospital technology not sufficiently integrated with Uninterruptible Power Supply (UPS) systems

Source: Engineered Systems Magazine
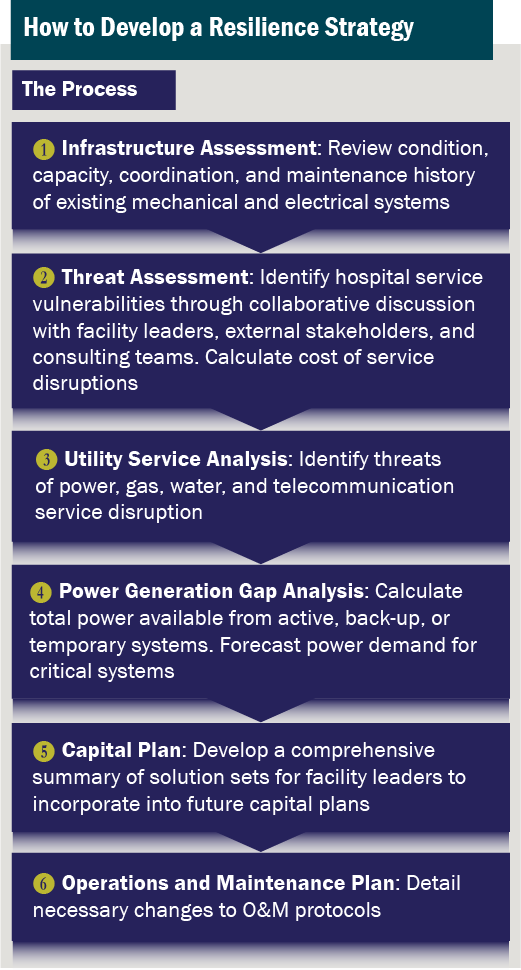
Steps to Develop a Resilience Strategy
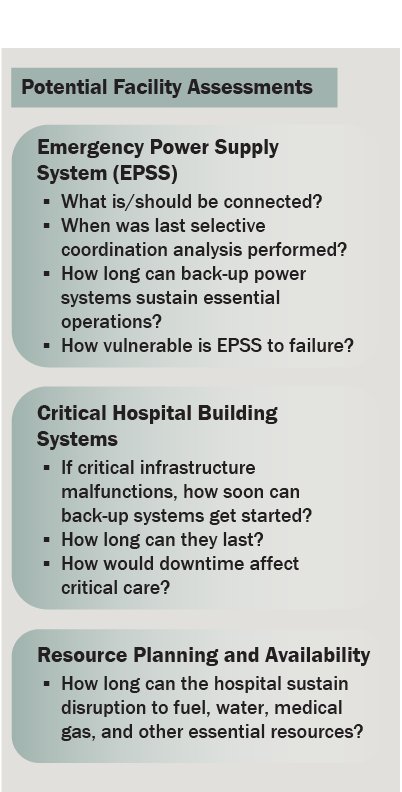
Healthcare systems can bolster disaster readiness through a series of self-assessments, identifying actionable short- and long-term measures to overcome major infrastructure vulnerabilities.
- Infrastructure Assessment
Reviews the condition, capacity, coordination, and maintenance histories of existing mechanical and electrical systems. Identifies whether major infrastructure systems, such as chilled water systems and telecommunication rooms, are connected to back-up power supplies or UPS devices.
- Threat Assessment
Identifies hospital service vulnerabilities through collaborative discussion with facility leaders, external stakeholders, and consulting teams, calculating potential cost of service disruptions.
- Utility Service Analysis
Assesses risk of external utility disruption, such as power, gas, water or telecommunication outages. Requires collaboration with utility representatives to gauge provider’s infrastructure conditions and resilience plans.
- Power Generation Gap Analysis
Calculates power available from active or back-up systems, forecasting total supplies, and to what extent a hospital can meet demand of critical systems.
- Disaster Recovery Plan
Anticipates how to resume operations following disruption to critical infrastructure whether through temporary solutions, modular systems, or start-up procedures.
- Facility Standards Analysis
Reviews relevant codes, regulations and standards, identifying changes in facility design standards necessary to address emerging threats and infrastructure vulnerabilities.
- Sustainability Initiatives
Identifies emission-reduction or resource-efficiency solutions that would not undermine the reliability and resilience of critical infrastructure system operations.
Potential Resilience Improvements
Resilience assessment should involve 360-degree reviews of critical infrastructure systems. Done effectively, findings can position facility leaders to develop the solutions sets best suited for a particular hospital campus. The following are examples of proactive resilience measures.
Eliminate Risk of Single Point of Failure
Hospitals can expand infrastructure system resilience by installing one more unit or component than necessary for normal operations. Additional equipment may be installed for back-up heating, ventilation and air conditioning (HVAC) systems, transfer switches, electric panels, or other critical infrastructure.
Incorporating this “N+1” approach prevents risks of downtime if an individual piece of equipment fails, supplies become unavailable, or back-up supplies are necessary over a prolonged period.
Source: Essential Hospitals Institute
Enhance Back-Up Power Resilience
Emergency power strategies depend on each hospital’s energy load, access to fuel supplies, and temporary equipment options. Resilience measures may include:
- Paralleling additional generators
If a unit fails, back-up loads are redistributed among remaining generators.
- Procuring stand-by power
Portable generators can provide supplemental power, provided contractors can overcome logistical challenges during a disaster or fuel shortage.
- Installing an outdoor docking station
Permanent connections facilitate adding portable generators to the hospital’s electrical power distribution system.
- Establishing an independent microgrid
During an outage, on-campus district energy solutions can deliver power to critical facilities. Distributed energy resources include solar photovoltaics (PV), combined heat and power (CHP), thermal storage, battery energy storage systems (BESS), or fuel cells.
Safeguard Technology Systems
UPS redundancy can help maintain critical loads, avoiding reliance on a single unit. System reliability depends on proper testing and maintenance, potentially through a Service Level Agreement (SLA). An alert and event-monitoring system can identify and address UPS anomalies before critical systems lose power.
Going Beyond Code — from Luxury to Necessity
Beyond-code emergency preparedness upgrades were once considered luxuries. Nowadays — in light of growing threats of extreme weather, utility outages, and supply chain disruptions — redundant back-up systems are too important to overlook.
Hospitals must act proactively and prioritize the resilience strategies most practical and impactful for their unique circumstances. By revising facility standards and integrating contingency planning throughout capital programs and maintenance protocols, healthcare leaders can protect their facilities against potentially dangerous infrastructure vulnerabilities and, in the process, demonstrate to the surrounding community that their hospital campus can be counted on — no matter what the future brings.
Burns partners with our healthcare clients to develop resilience plans and to implement facility improvements that maintain continuity of critical infrastructure throughout a wide range of disaster scenarios. Contact us for more information on Burns’ hospital resilience strategies.


