Submetering Tools More Efficiently Diagnose Hospital Energy Conditions
As hospitals grapple with post-pandemic revenue shortfalls and rising expenses, evidence-based cost management strategies will play an increasingly important role in the industry’s financial recovery.
Modern U.S. hospitals require huge amounts of energy. A lack of insights into consumption trends can leave facility managers uncertain how to best remedy inefficient use of electricity, gas, or steam utilities.
By tracking both facility-specific and campus-wide energy consumption, hospitals have greater visibility into their most inefficient building systems. Comprehensive, transparent system-performance data can help improve capital-improvement decisions, target energy-conservation measures, and assist maintenance staff proactively resolve system failures.
Intensive care with intensive energy
U.S. hospitals use more than double the amount of energy, measured per square foot, than comparably sized commercial buildings.
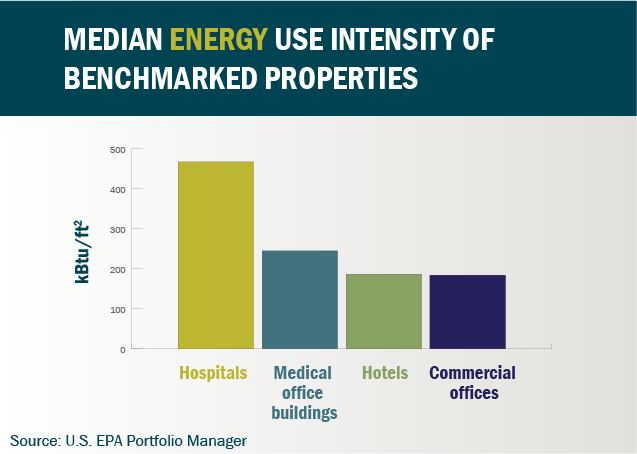
High energy-intensity levels are due to multiple factors:
- Hospitals operate around-the-clock, accommodating thousands of occupants every day.
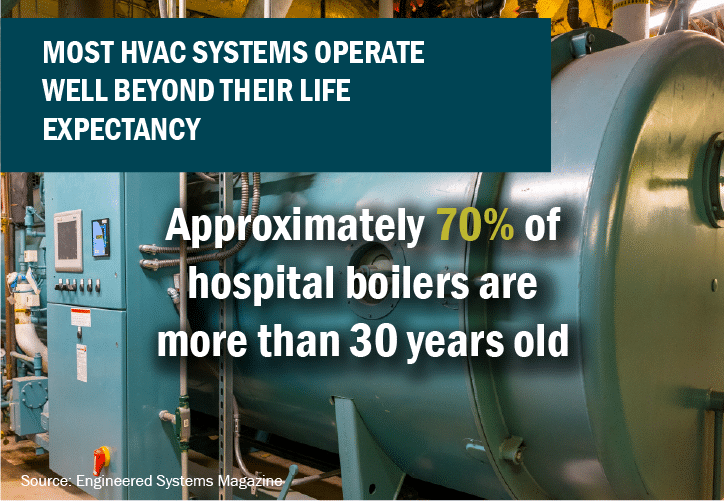
- Many rely on inefficient heating, ventilation and air conditioning (HVAC) equipment, maintained well past their useful life expectancy.
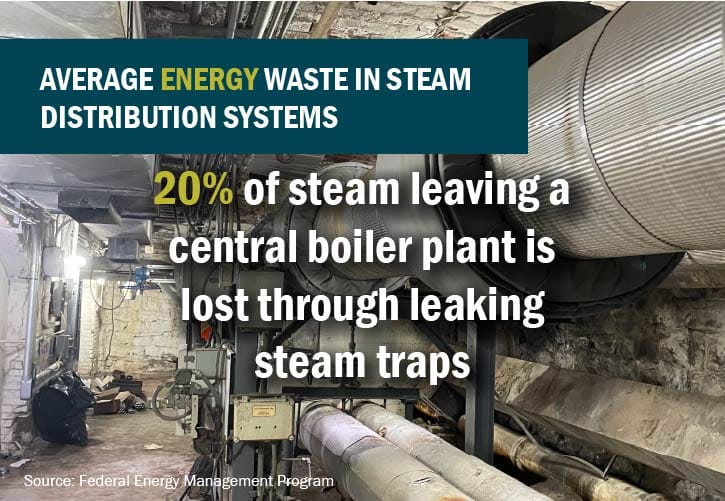
- Left unaddressed, steam distribution systems suffer from frequently clogged steam traps, leading to significant energy waste.
- More-stringent ventilation standards drive up energy consumption.
- Frequent and heavy use of energy-intensive medical, sterilization, and laundry equipment.
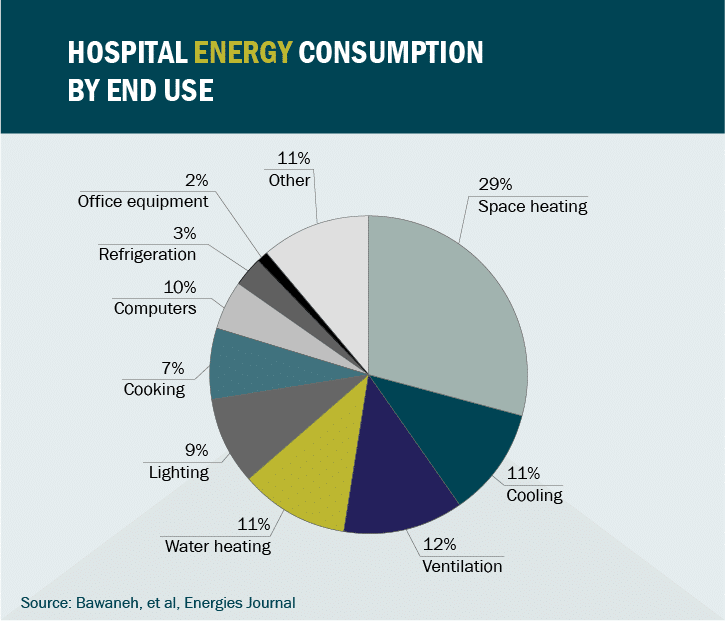
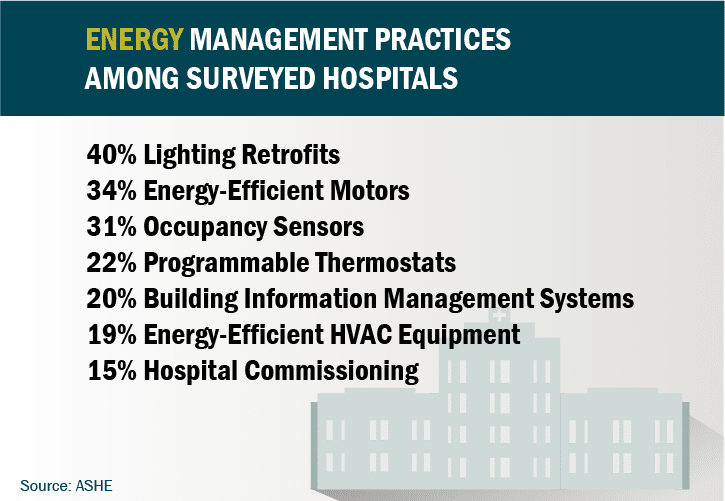
To improve hospital energy efficiency, an effective first step is to establish a baseline of facility-wide energy use. Thousands of U.S. hospitals record energy and water consumption through the U.S. Environmental Protection Agency’s Portfolio Manager. The database allows facility managers to compare energy performance with similar healthcare buildings.
Energy performance benchmarking can be a tool to focus investments on the energy-related projects that offer greatest savings potential. For hospitals that have already successfully implemented energy-saving projects, benchmarking assists with identifying replicable best practices.
The quality of a benchmarking analysis, however, depends largely on the granularity of energy-consumption data. Facility managers can identify the root causes of energy waste when they have access to advanced submeters, installed for specific energy measurements, better targeting their energy-conservation measures.
Hospital submetering benefits
Traditional flow meters track facility-wide consumption of electric, gas, steam and water utilities, mostly for billing purposes. The single-meter approach generally simplifies payment processes, especially on campuses where consumption can vary significantly between buildings. Yet hospitals that rely upon a single meter lack access to real-time insights that reveal energy consumption patterns.
Advanced, “smart” meters track consumption over time, providing valuable metrics on seasonal or hourly consumption. Advanced meters can integrate with building management systems, alerting facility managers when consumption spikes unexpectedly. These meters also enable better management of peak-consumption electricity charges and allow hospitals to participate in demand-response programs.
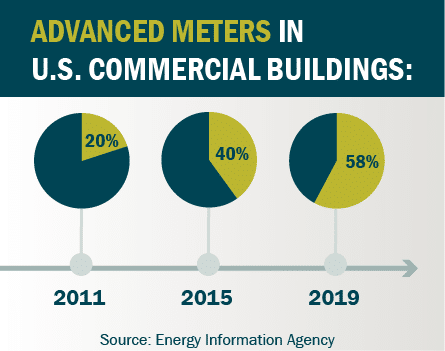
To identify utility consumption trends for specific facilities across a campus or for specific systems within a building, hospitals need to install multiple advanced meters. This strategy, known as submetering, tracks energy consumed by specific building spaces, medical equipment, or HVAC systems.
Facility managers who crunch this data can develop “after-the-meter” analyses that help with targeting the energy-efficiency retrofit strategies that generate greatest financial returns.
Other reasons hospitals install submeters:
- Allocate utility consumption to specific tenants or departments, billing for their respective usage.
- Simplify the process to recover federally funded research expenses related to utilities.
- Demonstrate energy savings when applying for rebates through utility energy-conservation programs.
- Improve equipment or HVAC-system commissioning practices based on real-time consumption trends.
Cost-effective submetering strategies
Submetering design varies according to each hospital’s energy-management goals. The level and type of desired energy usage data will determine submeter quantity and locations.
To track electrical consumption, submeter placement options include:
- Electrical switchboards,
- Sub-distribution systems,
- Multiple points within a panel system, or
- Automatic transfer switches.
Facilities that have already installed a building automation system are presented a great platform from which to log energy-use data. By also submetering mechanical systems, facility managers can identify maintenance issues prior to an equipment failure. For example, surveillance of chiller energy consumption could reveal the need to provide annual tube cleaning.
Certain HVAC systems may be metered by the following tracking options:
- Heat-generation equipment can be measured through flow meters at the gas or oil valve train, or tracked from the electrical current sensor.
- Ventilation equipment and pumps can be monitored by reading the current sensing transducers or from variable frequency drive motor starters.
Submeters can track all hospital utilities for any space or system. An effective strategy justifies each meter installation, delivering cost savings that exceed the submeter’s costs. Gas and steam submeters tend to be more expensive and often prove more complicated to install. Beyond installation expenses, submeter costs include:
- Operational and maintenance expenses for periodic calibration, testing, and communication fees.
- Staff time dedicated to analysis of the submeter data.
- Auxiliary systems such as a Water Air Gas Electricity Steam (WAGES) panel.
Alternatively, energy-intensive steam distribution systems can be monitored through active steam-trap surveillance systems. Automatic steam trap monitoring through fault detection and diagnostics (FDD) can:
- Identify incidents of energy waste, sending notifications to hospital facility staff when a steam trap fails.
- Replace the manual monitoring processes usually deployed at hospitals, avoiding the lengthy amount of time often required to locate costly system failures.
Quality healthcare through energy efficiency
A surgical approach to hospital energy management begins with a diagnostic evaluation of facility-wide utility systems.
Submeters can help reveal the information necessary to diagnose system failures. Or — if inefficient building systems are otherwise fully functioning — submeters provide evidence-based rationale to motivate hospital administrators that upfront costs of an energy-efficiency upgrade would deliver worthwhile financial returns.
Widespread application of advanced submeters can be expensive. But technology advances continue to lower their costs. Strategic placement of the appropriate submeter within the most effective application can cost-effectively enable hospitals to reduce energy consumption and lower their overall carbon footprint.
Ultimately, submetering strategies can help hospitals deliver exceptional patient care. By lowering operating costs, projects that successfully reduce energy expenses free up financial resources that can instead be allocated toward patient amenities.


